Registos clínicos electrónicos: diferenças entre revisões
| Linha 63: | Linha 63: | ||
** Recolha e interpretação de imagem | ** Recolha e interpretação de imagem | ||
Quem deveria recolher os dados dos pacientes? | === Quem deveria recolher os dados dos pacientes? === | ||
{| class="wikitable" | {| class="wikitable" | ||
Revisão das 16h35min de 18 de fevereiro de 2016
Os registos clínicos / prontuários electrónicos são uma parte fundamental do conjuntos dos sistemas de informação de qualquer instituição de saúde.
São uma nova forma de encarar os Registos Clínicos, e devem ser capazes de permitir uma evolução clara em relação aos Registos Clínicos em Papel.
Definições
- Electronic medical record
- A general term describing computer-based patient record systems. It is sometimes extended to include other functions like order entry for medications and tests, amongst other common functions. What does an electronic medical record (EMR) do? For many it is much more than an electronic replacement of existing paper systems. The EMR can start to actively support clinical care by providing a wide variety of information services. However, it is hard to understand what information is really important to clínical care, and what is simply occasionaly desirable.“ [1]
Importância
“Health-care organizations, finding that they do not have adequate systems for answering questions crucial to strategic planning and for remaining competitive with other provider groups, are looking to information technologies for help. Many institutions are developing integrated clinical workstations, which provide a single point of entry for access to patient-related, administrative, and research information. At the heart of the evolving clinical workstation lies the medical record in a new incarnation: electronic, accessible, confidential, secure, acceptable to clinicians and patients, and integrated with other, non-patient-specific information.”[2]
Pressões para o uso de registos electrónicos
- A necessidade do uso de dados de pacientes tem aumentado
- Maior acesso às TIC para o suporte aos RCEs
- Os computadores têm sido aceites como ferramenta para aumentar a eficiência em todas as facetas do nosso dia-a-dia
- Factores demográficos como o envelhecimento e mobilidade permanente, cria uma grande pressão para registos clínicos capazes de gerir grandes quantidades de informação
- A pressão para fazer reformas na prestação de cuidados aumenta, sendo a automação de registos clínicos fundamental para estas
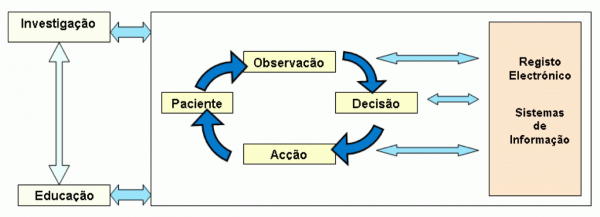
Ciclo diagnóstico-terapêutica e o RCE
Estruturação da informação
A estruturação de informação possibilita:
- normalização da informação
- fazer tratamento dos dados clínicos
- ter mecanismos de alerta
- sistemas de apoio à decisão clínica
- avaliar a prestação de cuidados
- fazer investigação clínica
Introdução de dados
Para facilitar a introdução dos dados podem-se criar mecanismos de:
- alerta para correcção de erros de introdução
- tecnologias touch-based ou pen-based
- sistemas de reconhecimento de voz
- sistemas de processamento de linguagem natural
Utilizadores envolvidos e métodos de recolha de dados
- Pacientes:
- Questionários
- Diários
- Formulários
- Touch-screens
- Web Browser
- Telefone (phone menu system)
- Clínicos
- Escrita em Formulários
- Point and click e Touch-Screens
- Ditar e transcrever
- Reconhecimento de voz
- Recolha automática
- Sinal
- Recolha e interpretação de imagem
Quem deveria recolher os dados dos pacientes?
| Habilidades Clinicas | Tempo | Disponibilidade para seguir uma checklist | |
|---|---|---|---|
| Médico | +++ | - | - |
| Enfermeiro | ++ | + | + |
| Técnico triagem por telefone | + | ++ | ++ |
| Paciente | - | +++ | ++++ |
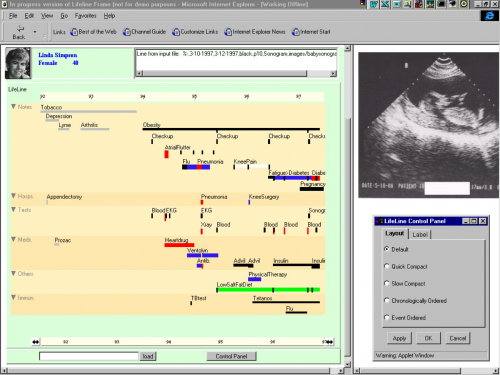
Visualização de informação
A informação clínica pode ser mostrada de forma integrada, embora:
- as fontes de informação possam ser diferentes
- usem diferentes tecnologias e formatos
- visualização pode ser dinâmica e organizada de diferentes formas
Problemas registos electrónicos
- Introdução de dados inicialmente mais lenta
- Necessitam de formação específica dos profissionais de saúde
- Consumo de recursos iniciais na educação e treino
- Obriga a actualização de conhecimentos constante
- Pouca flexibilidade nas restrições impostas ao acesso da informação (se a pessoa que tem acesso não está disponível o acesso não se realiza)
- Dão pouca liberdade no estilo de escrita dos relatórios
- Não podem ser transportados facilmente de um lado para outro
- Problemas de quebra de segurança
Trabalhos científicos sobre registos clínicos
Impacto dos RCE
- Clinical Information Technologies and Inpatient Outcomes - A Multiple Hospital Study [3]
- Background: Despite speculation that clinical information technologies will improve clinical and financial outcomes, few studies have examined this relationship in a large number of hospitals.
- Methods: We conducted a cross-sectional study of urban hospitals in Texas using the Clinical Information Technology Assessment Tool, which measures a hospital's level of automation based on physician interactions with the information system. After adjustment for potential confounders, we examined whether greater automation of hospital information was associated with reduced rates of inpatient mortality, complications, costs, and length of stay for 167 233 patients older than 50 years admitted to responding hospitals between December 1, 2005, and May 30, 2006.
- Results: We received a sufficient number of responses from 41 of 72 hospitals (58%). For all medical conditions studied, a 10-point increase in the automation of notes and records was associated with a 15% decrease in the adjusted odds of fatal hospitalizations (0.85; 95% confidence interval, 0.74-0.97). Higher scores in order entry were associated with 9% and 55% decreases in the adjusted odds of death for myocardial infarction and coronary artery bypass graft procedures, respectively. For all causes of hospitalization, higher scores in decision support were associated with a 16% decrease in the adjusted odds of complications (0.84; 95% confidence interval, 0.79-0.90). Higher scores on test results, order entry, and decision support were associated with lower costs for all hospital admissions (–$110, –$132, and –$538, respectively; P < .05).
- Conclusion: Hospitals with automated notes and records, order entry, and clinical decision support had fewer complications, lower mortality rates, and lower costs.
Impactos negativos
- Vets exposed to wrong drug doses [4]
- Patients at VA health centers were given incorrect doses of drugs, had needed treatments delayed and may have been exposed to other medical errors due to the glitches that showed faulty displays of their electronic health records, according to internal documents obtained by the Associated Press under the Freedom of Information Act.
- The glitches, which began in August and lingered until last month, were not disclosed to patients by the VA even though they sometimes involved prolonged infusions for drugs such as blood-thinning heparin, which can be life-threatening in excessive doses. In one case, a patient having chest pains at the VA medical center in Durham, N.C., was given heparin for 11 hours longer than necessary as doctors sought to rule out a heart attack.
- The VA's recent glitches involved medical data - vital signs, lab results, active meds - that sometimes popped up under another patient's name on the computer screen. Records also failed to clearly display a doctor's stop order for a treatment, leading to reported cases of unnecessary doses of intravenous drugs such as heparin.
- The goal of electronic medical records nationwide is to help avert millions of medical mistakes attributed in part to paper systems, such as poorly written prescriptions. But health-care experts say the VA's problems illustrate the need for close monitoring.
Referências
- ↑ “In Guide to Medical Informatics” - Enrico Coiera
- ↑ “The evolution of Electronic Medical Records” – EH Shortliffe
- ↑ Ruben Amarasingham, MD, MBA; Laura Plantinga, ScM; Marie Diener-West, PhD; Darrell J. Gaskin, PhD; Neil R. Powe, MD, MPH, MBA . Clinical Information Technologies and Inpatient Outcomes - A Multiple Hospital Study. Arch Intern Med. 2009;169(2):108-114.
- ↑ Hope Yen. Vets exposed to wrong drug doses. Jan. 15, 2009 Associated Press